What is Endoscopic Ultrasound (EUS)?
Endoscopic ultrasound (EUS) is a minimally invasive endoscopic technique which allows the doctor (endoscopist) to obtain detailed images of the pancreas. EUS provides the endoscopist with information additional to that obtained with CT or MRI imaging. It can be used to take needle biopsies from abnormal areas of the pancreas, avoiding exploratory surgery or can be used to take sample fluid from a pancreatic cyst.
Why is Endoscopic Ultrasound (EUS) important to you?
Endoscopic Ultrasound (EUS) brings imaging technologies to the forefront of advancing patient care. Going beyond the layers, the colors of sound bring to life information you need to make confident decisions with unparalleled accuracy.
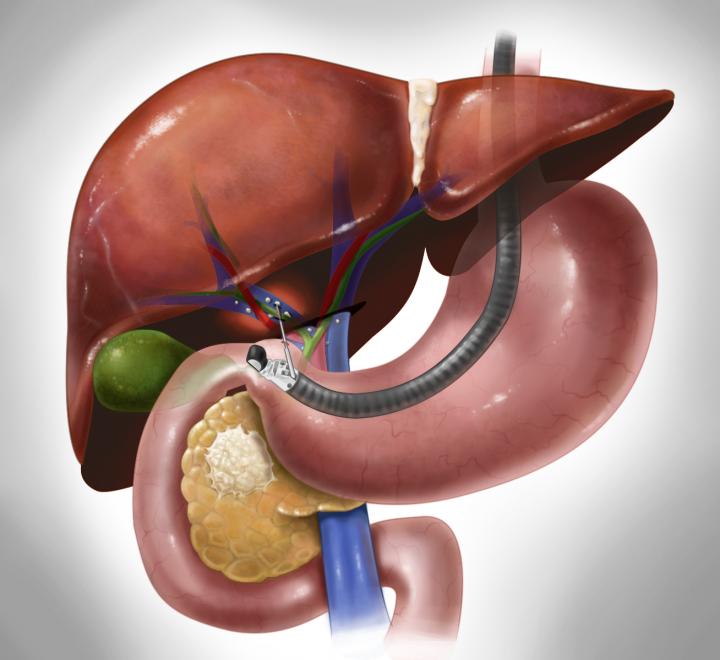
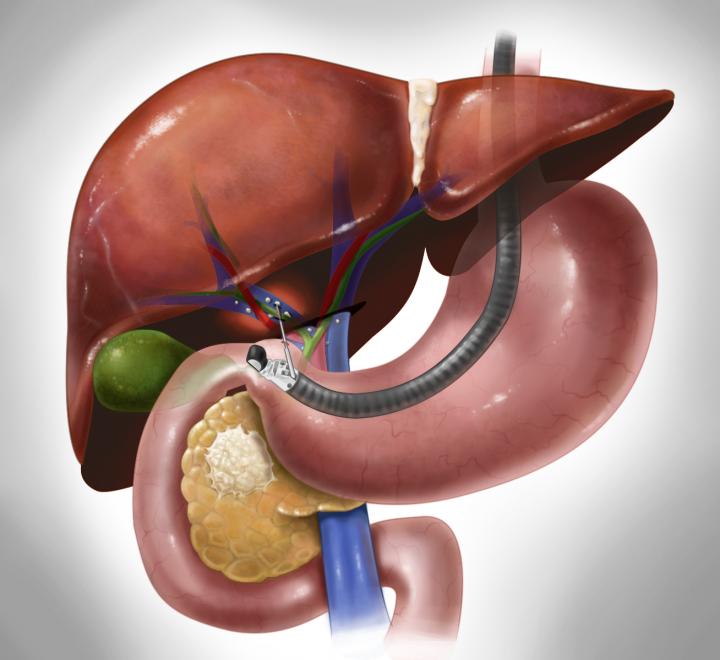
How is EUS performed?
A thin, flexible tube (endoscope) is passed through the mouth and into the stomach and duodenum or rectum. The tip of the endoscope contains a built in miniature ultrasound probe which emits sound waves. These sound waves pass through the lining of the stomach and duodenum creating a visual image of the pancreas and surrounding tissue. EUS can be used to obtain a needle biopsy of the pancreas or to sample fluid in a pancreatic cyst. This is done by passing a very thin needle from the endoscope into the pancreas under continuous ultrasound monitoring. This technique is called EUS-fine needle aspiration (EUS-FNA) and does not hurt.
Where is EUS performed?
Procedures are performed either in the morning or afternoon. As you will be receiving intravenous (IV) sedation you will not be allowed to drive after the procedure. It is important that you have a companion (family member or friend) to take you home and plan to have someone stay with you at home after the examination as sedatives can affect your judgement and reflexes for up to twenty four hours.
Will I be awake for the procedure?
The EUS procedure is performed using intravenous sedatives which help you relax. Depending on the sedation used, you may not remember the procedure. Most patients consider the procedure only slightly uncomfortable, while some fall asleep during it.
How long does the procedure take and what happens afterwards?
The actual procedure takes approximately 30-60 minutes. Most patients are discharged 1-2 hours after they arrive. Following the procedure, you will be monitored in the recovery area until the effects of the sedation have worn off. You will be able to eat after the procedure.
Will I be admitted for the procedure?
The procedure is usually performed as an outpatient. Most people are able to go home one to two hours within completion of the procedure.
When will I be given the results of the EUS?
Your endoscopist will usually be able to give you the preliminary results of the EUS on the same day as the procedure. If an EUS-FNA has been performed, these results take between fi e to seven days to return. Follow up in GI clinic to go over results and plan of care.
What are the possible complications associated with EUS?
EUS is a very safe procedure and although complications occur, they are rare when doctors with specialized training and experience perform the EUS examination. You may have a sore throat which usually resolves within a day or two. Sometimes people feel a little bloated due to the air inserted by the instrument. Other potential but uncommon complications of EUS include a reaction to the sedatives used, aspiration of stomach contents into your lungs, and complications affecting the heart or lungs. One major, but very uncommon complication of EUS is where there is a tear in the lining of the stomach or duodenum, called a perforation. This is very rare but can require surgery to repair the tear. If an EUS-FNA is performed, where a needle is passed into the pancreas to take a sample, there is a small risk of bleeding, pancreatitis or infection. To decrease the risk of infection, we routinely prescribe antibiotics for patients in whom EUSFNA was performed on a pancreatic cyst.
What are the benefits for using Endoscopic Ultrasound (EUS)?
• No radiation.
• Staging of cancers of the esophagus, stomach, pancreas and rectum.
• Evaluating chronic pancreatitis and other masses or cysts of the pancreas.
• Studying the bile duct abnormalities including stones in the bile duct or gallbladder, or studying tumors within the bile duct, gallbladder, or liver.
• Studying the muscles of the lower rectum and anal canal in evaluating reasons for fecal incontinenece
• Studying submucosal leasions such as nodules or bumps that may be hiding in the intestinal wall covered by normal appearing lining of the intestinal tract.