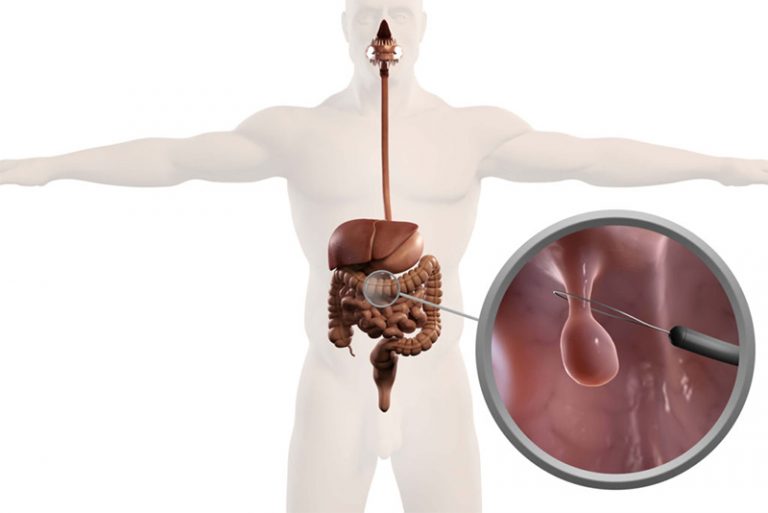
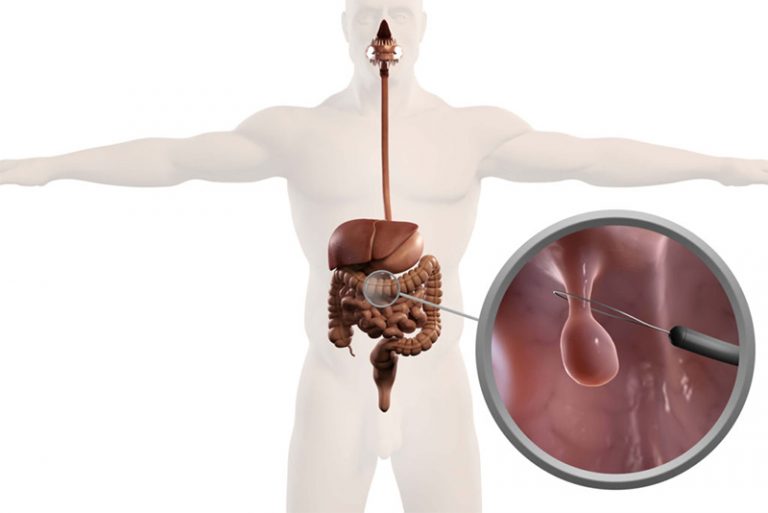
ENDOSCOPIC MUCOSAL RESECTION (EMR)
Endoscopic mucosal resection is performed with a long, narrow tube equipped with a light, video camera and other instruments. During endoscopic mucosal resection of the upper digestive tract, the tube (endoscope) is passed down your throat to reach an abnormality in your esophagus, stomach or upper part of the small intestine (duodenum).
Why is Endoscopic Mucosal Resection Done:
Endoscopic mucosal resection is a less invasive alternative to surgery for removing abnormal tissues from the lining of the digestive tract. These tissues may be:
- Early-stage cancer
- Precancerous lesions, abnormal tissues that may become cancerous
Endoscopic mucosal resection is usually performed by a specialist in digestive system disorders (gastroenterologist) who has expertise in this technique.
What are the risk?
Risks of the endoscopic mucosal resection include:
- Bleeding. Bleeding, the most common complication, can often be detected and corrected during the procedure.
- Puncture (perforation). There is a slight risk of a puncture through the wall of the digestive tract. The risk of perforation may depend on the size and location of the lesion that’s removed.
- Narrowing of the esophagus. For people who have endoscopic mucosal resection of the esophagus, there is some risk of narrowing of the esophagus (esophageal stricture), particularly if a lesion encircles the circumference or nearly the entire circumference of the esophagus. Removing the lesion can lead to scarring that narrows the esophagus, a condition that may lead to difficulty swallowing and require further treatment.
Call your doctor or get emergency care if you experience any of the following signs or symptoms after undergoing endoscopic mucosal resection:
- Fever
- Chills
- Vomiting
- Black stool
- Bright red blood in the stool
- Chest or abdominal pain
- Shortness of breath
- Fainting
How you prepare:
Before you have endoscopic mucosal resection, you’ll be asked to provide the following information:
- All of the prescription medications, over-the-counter drugs and dietary supplements you take — particularly diabetes medications and blood-thinning drugs, including aspirin
- Doses of each medication
- Drug allergies
- All medical conditions, including heart disease, lung disease, diabetes and blood-clotting disorders
Your doctor may make changes to your medication routine, such as temporarily stopping some blood-thinning medications.
Before the procedure:
You’ll receive written instructions about what to do starting the day before the procedure. These instructions may vary depending on the location of the lesion or lesions being removed. In general, the instructions will likely include the following:
- Restricted diet. The day before the procedure, your diet may be limited to clear liquids, such as water, broth, and tea or coffee without milk or cream.
- Fasting. You’ll be instructed when to begin fasting. You may not be able to eat, drink or smoke at all after midnight the day before the procedure.
- Cleaning the colon. If the procedure involves the colon, you’ll likely use a liquid laxative or an over-the-counter enema kit to empty your bowels completely and clean your colon.
You’ll also sign an informed consent document giving your doctor permission to perform the procedure after the risks and benefits have been explained to you.
Travel arrangements:
Because endoscopic mucosal resection is almost always performed as an outpatient procedure, you’ll likely go home the same day. However, because of sedation used during the procedure, you’ll need to make plans to have someone take you home after you’re released from the hospital or clinic.
What you can expect:
There are a few different versions of endoscopic mucosal resection. Ask your gastroenterologist about how your procedure will be performed. A common approach includes these steps:
- Insertion of the endoscope and guiding the tip to the area of concern
- Injecting a fluid under a lesion to create a kind of cushion between the lesion and healthy tissue underneath it
- Applying gentle suction to the lesion to lift it up
- Snaring and cutting the lesion to separate it from surrounding healthy tissue
- Removing the abnormal tissue from your body
- Marking the area with ink (tattoo) so that it can be found again with future endoscopic exams
During the procedure:
During an endoscopic mucosal resection, you can expect the following:
- Your role. You’ll be asked to change into a gown before the procedure. During the procedure, you’ll lie on your side on a cushioned table.
- Sedation. You’ll be sedated during the procedure. This may be moderate sedation that causes you to be relaxed and drowsy. If this is the case, you may feel some slight movement or pressure during the procedure, but you shouldn’t feel any pain. Or you may be heavily sedated and not be alert at all during the procedure. You can discuss with your gastroenterologist which option is appropriate for you.
- Monitoring. The gastroenterologist performing the procedure will be assisted by nurses or other professionals, who will monitor your heart rate, blood pressure, blood oxygen level and comfort.
After the procedure:
After the procedure, you’ll remain in a recovery room until most of the effect of the sedative has worn off. You’ll receive written instructions about when you can start eating and drinking and when you can resume normal activities. You’ll be advised not to do any of the following activities until the next day:
- Drive
- Return to work
- Make important decisions
Relatively mild side effects may occur within the first 24 hours after the procedure. These may include:
- Reactions to the sedative. The drugs used to sedate you may continue to cause drowsiness and may cause nausea and vomiting.
- Sore throat. If the endoscope was guided down your esophagus, you may experience a sore throat.
- Gas or cramps. A small amount of air may have been pumped into your digestive system to make it more accessible. This can result in gas, bloating or cramps after the procedure.
You’ll also receive written instructions about when to call your doctor or get emergency care after the procedure. The following signs or symptoms may indicate a serious complication from endoscopic mucosal resection:
- Fever
- Chills
- Vomiting
- Black stool
- Bright red blood in the stool
- Chest or abdominal pain
- Shortness of breath
- Fainting
Results
You’ll likely have a follow-up appointment with the gastroenterologist to discuss the outcome of your endoscopic mucosal resection and laboratory tests performed on lesion samples. Questions to ask include the following:
- Were you able to remove all abnormal tissues?
- What were the results of the laboratory tests? Were any of the tissues cancerous?
- Do I need to see a cancer specialist (oncologist)?
- If the tissues are cancerous, will I need additional treatments?
- How will you monitor my condition?
Follow-up exams:
Typically, a follow-up exam is performed six to 12 months after your procedure to be sure the entire lesion was removed. Depending on what is found, your doctor will advise you when further examinations are necessary.
An exam will likely include a visual inspection with the use of an endoscope. Your doctor may mark the area of the removed lesion with ink (tattoo) so that when follow-up endoscopy is performed, he or she can be sure the lesion was removed completely.